It is well documented that the neuropathology of Alzheimer’s disease is associated with activated microglia. Microglia, the resident macrophages of the brain, are normally quiescent or down-regulated when compared to other tissue macrophages, but in chronic neurodegeneration in diseases such as Alzheimer’s disease, Parkinson’s disease and prion disease they are activated and express molecules not seen on the normal resting cells.
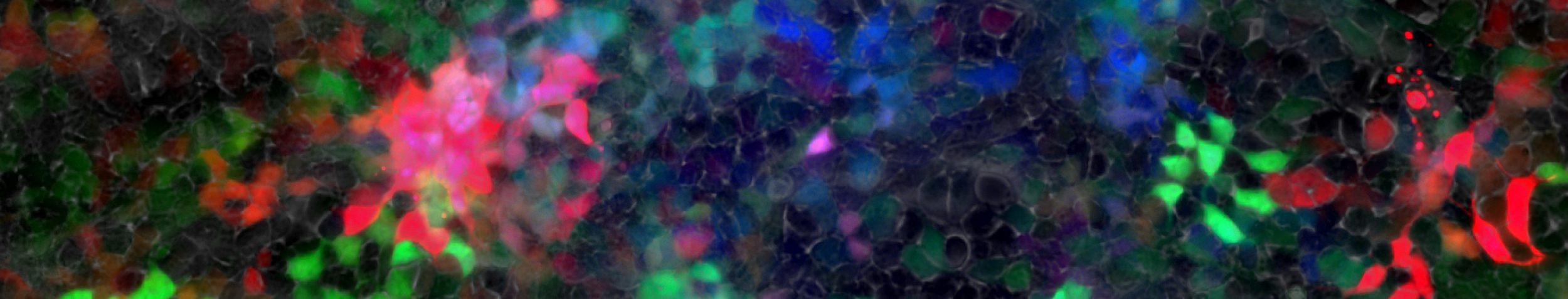
It is unclear whether they contribute to the disease process, or are simply activated as a consequence of the tissue degeneration. We are investigating the microglia activation in a model of prion disease, mouse scrapie. In this disease the microglia become activated prior to the onset of clinical signs of the disease, but are associated with synaptic loss the earliest neuronal pathology in this and other chronic neurodegenerative diseases.
We have investigated the inflammatory mediators and cytokines that are produced by the activated microglia in advanced stages of pathology. Unlike in an acute challenge to the brain, in the prion diseased brain there is little evidence of a typical pro-inflammatory cytokine response but there are increased levels of prostaglandins and TGF-b. Pioneering research from Prof V. Hugh Perry and Prof Clive Holmes found that these microglia may be switched from this anti-inflammatory phenotype to a pro-inflammatory phenotype by systemic infection or inflammation. This switch in phenotype is associated with exaggerated sickness behaviour, exaggerated cytokine synthesis and enhanced neuronal degeneration. These pre-clinical findings have been translated into the clinical setting. Prof Clive Holmes and colleagues have shown that systemic inflammation accelerates cognitive decline in patients with Alzheimer’s disease.